Where is the norm and where is it no longer?
We will try to understand what a BAR is and how it differs from simple mood swings. After all, joy and sadness are normal human emotions, and it's perfectly normal to experience them.
Emotions and the mood of the person is a mobile part of the human psyche, in the norm they are constantly changing, and the strength and duration of these emotions is directly related to the events that caused them and the temperament of man - someone reacts very violently to any change and his mood is constantly changing, and someone is very calm, and his mood is not particularly subject to change.
Throughout life we experience many different emotions: Positive: pleasure, excitement, joy, sympathy, tenderness, surprise, curiosity, etc. And negative: disgust, resentment, anger, irritation, anxiety, anger, sadness, fear, despair, etc.
For example, sadness is an emotional response to loss, defeat, or trouble. And joy is a response to pleasant events. Aggression and anger are experienced when we are threatened by something.
If the strength and duration of the emotional response is consistent with the situation that caused it, we are talking about normal human emotion. Regardless of strength, normal emotional reactions fade over time, even in a situation of grief or great joy, a person returns to a balanced state.

If, however, a person gets stuck in this or that state for a long time, if the strength and duration of emotions are no longer related to situations and life events, then we are talking about a mood disorder. In affective disorders, emotions are characterized by duration and strength. They lose their connection to the event, become disproportionate to them, and take on a life of their own.
What do people with bipolar disorder have in common?
People with affective disorder often have similar temperament characteristics that show up even before the illness. For example, people with bipolar affective disorder can be found with hyperthymic or cycloid accentuations of character.
A character accentuation is a variant of the norm, and a person who has an accentuation has his or her own characteristics. For example, a person with hyperthematic accentuation constantly lives in high spirits, even in difficult situations, he does not lose heart, such as Dr. Livesey from the cartoon Treasure Island, Jack Sparrow from Pirates of the Caribbean or Winnie the Pooh from an old Soviet cartoon. Such people are full of energy, cheerful and curious most of the time.
A person with cycloid accentuation is a person who was Winnie the Pooh yesterday and is now a donkey IA. When he was Winnie the Pooh, he made appointments with friends, started many errands, and then his mood changed and he canceled everything and stayed home.
People with cycloid accentuations are often suspected of having BAR, and they do have unexplained ups and downs in their moods - today they are happy, and tomorrow they are just sad.
Yet cycloid accentuation is far from a BAR.
People with BAR have a number of other characteristics that can be noticed:
"These are people generally mild, good-natured, inclined to sociability, with rounded mental movements, in whom nothing abrupt, impulsive, incomprehensible is observed. They are very prone to blend into their environment, or, as Bleuler says, very synthonic. All their actions are understandable, precisely as people of the environment; in this connection they seldom show any anti-social tendencies." V.A. Gilarovsky, Psychiatry. A Manual for Physicians and Students, 1954
Basic symptoms and manifestations of bipolar disorder
Conditions such as mania and melancholy have been known to people for centuries, and it was already noted that these conditions sometimes occur in the same people. Melancholy was described in the school of Hippocrates as early as the 5th century B.C. And the description of mania can be found in another Greek physician, Areteus of Cappadocia, a description he made 2,000 years ago:
"Some patients with mania are cheerful; they laugh, play, dance day and night; they stroll through the market sometimes with a wreath on their head, as if they had won the games: such patients do not cause unnecessary trouble for relatives. However, there are also those who lapse into mania... The manifestations of mania are innumerable. Some people who fall into mania, of those who are intelligent and well educated, are engaged in astronomy, despite the fact that previously it has never studied, with enthusiastic self-indulgence indulge in philosophical discourse, as a gift of the muses consider poetic ability." Janusz Rybakowski, Faces of Manic Depressive Disorder
In the middle of the 19th century, the disease was described almost simultaneously by two researchers, J. P. Falreux under the name "circular psychosis" and J. G. F. Bayarger under the name "lunacy in two forms."
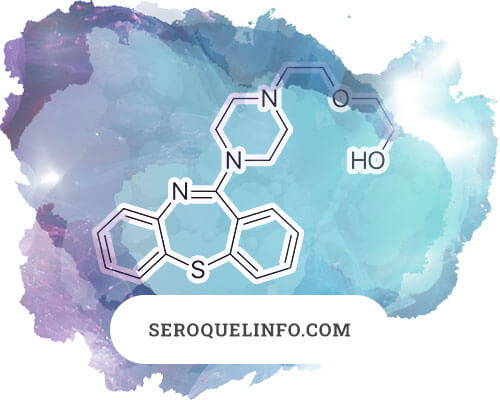
The foundation of the modern understanding of the disease was laid by Emile Kraepelin. In his 1899 textbook on psychiatry, he identified two main groups of mental disorders - "early dementia," which was later renamed schizophrenia, and "manic-depressive psychosis."
The name manic-depressive psychosis well reflected the essence of the disease, but, first, it implied the presence of psychosis, which does not always occur in IDD, and, second, it contributed to stigmatization.
The concept of MDP essentially included two disorders:
- What is now called recurrent depressive disorder.
- And bipolar affective disorder itself.
Bipolar affective disorder is a chronic mental illness categorized as a mood disorder. It manifests itself as episodes of subdepression, depression, hypomania, mania, and also mixed states.
Between episodes, the person usually completely recovers. The episodes are also called phases or bouts of illness, and the period of health between them is called - intermission, lucid interval or euthymia.
Even during these periods, however, many patients may remain or briefly exhibit some symptoms of bipolar disorder.
On average, depressive episodes last longer, from two weeks to a year, and account for the majority of all phases - about 80%. Manic episodes occur less frequently and last from a few days to 3 to 4 months. There are also mixed phases, which are manifested either in the simultaneous coexistence of symptoms of mania and depression, or in their rapid change. Mixed phases occur in about 30% of patients with BAR.
Some phases begin suddenly, some unfold gradually. In most cases, episodes of the disease begin in a person at the same time of year and follow the same script.
There are different types and forms of BAR, which I will discuss in the next article. The frequency and severity of episodes also varies. Some people may experience 2-3 episodes of the disease in a lifetime, while others have to deal with it several times a year. Some may be able to cope with minimal medical intervention, while others have to go to the hospital and take medications for the rest of their lives.
The three main types of bipolar disorder now include type 1 BIA, type 2 BIA, and cyclothymia.
Statistics
- The disease usually begins at a young age, up to 20 years old. It most often begins with depression - almost 90% of cases.
- The prevalence of BAR used to be thought to be 1-2%; over time, diagnosis has improved and milder cases that were previously off the radar of doctors have joined the main forms of bipolar disorder.
- Today, the prevalence of BAR 1 is thought to range from 0.7% to 1.6% and BAR 2 from 0.3% to 2%. The overall prevalence of bipolar spectrum disorder is 3 to 6.5%.
- The disorder is more common in women than in men, at a ratio of about 3:2.
- It is one of the most common causes of disability worldwide.
- Bipolar disorder shortens life by an average of nine years.
- Because of still poor diagnosis, people most often do not learn their diagnosis until 5 to 10 years after onset, which unfortunately complicates the course of the disease.
- Divorce rates for people with BAR are 2 to 3 times higher than for healthy people, people with BAR are twice as likely to have work problems, and are 5 times more likely to commit delinquency.
- 73% of patients with BAR are initially misdiagnosed, only to be correctly diagnosed 8 years later. 59% experience their first episode in childhood or adolescence.
- Women with BAR may lose 5 years of life, 12 years of normal health, and 14 years of social functioning.
- Between 20 and 60% of people with BAR have attempted suicide. (According to various studies).
The reasons for the development of BAR are not entirely clear, and it is likely that many different mechanisms are involved, probably genetic and biological factors play a role. Environment and psychosocial factors also influence the development of the disease.
The first phase of bipolar disorder, be it mania or depression, can be triggered by external events - stress, grief, mental trauma, illness. Afterwards, the connection with circumstances is lost, and phases most often arise by themselves, irrespective of events. But the person remains vulnerable to stress and external factors, and they may provoke a new or aggravate the current phase.
In the absence of timely diagnosis and treatment, concomitant psychiatric disorders can occur - alcohol or drug dependence, anxiety-phobic disorders, eating disorders, personality disorders and others. People with BAR are more likely than average to have some somatic diseases, such as diabetes, migraine, hypertension, cardiovascular disease, metabolic disorders, pain syndromes, etc.
BAR does not result in personality disorders, cognitive impairment, or any other. During intermissions or remissions, a person can be considered healthy. However, in the case of frequently relapsing phases, people often lose their jobs, social activities, etc.
To date, the criteria for mania and depression are fairly well defined, but classic episodes of bipolar disorder are not very common - in 37.8% of cases.
The frequency of episodes and the nature of remissions and exacerbations are quite varied, in general remissions tend to shorten with age, and depression becomes more frequent and longer after middle age.
In general, episodes of bipolar disorder can disorganize behavior, disrupt interpersonal relationships, and lead to conflicts at work and lawbreaking. In cases of frequent relapses, people lose the ability to live independently.
Depressive episode
Depression - In bipolar disorder, it is manifested by decreased mood, increased fatigue, and decreased interest in things that used to give pleasure. At the same time, self-esteem drops, thoughts of worthlessness and guilt arise, and sometimes there is a desire to die, as well as impaired appetite and sleep. To be diagnosed, the condition must last at least two weeks in a row.
Depressions tend to have a longer course than other phases of bipolar disorder (average duration about 6 months), although rarely more than a year (excluding elderly patients).
Depressive phases in general occur more frequently and account for 80% of all episodes.
"I felt myself crumpling under something much stronger than me; first my legs went weak at the ankles, then I lost the ability to control my knees, then my lower back began to crack from the strain, finally my shoulders went into hibernation, and I ended up curled up like a fetus, utterly devastated by this creature that was crushing me without any support at all. Its tentacles threatened to destroy my mind, my courage, my stomach, crush my bones, dry out my body. She gorged herself on me, even when I seemed to have nothing left to feed her." Andrew Solomon, Noon Demon
Depression, it's not about sadness, it's about the inability to feel joy. The inability to feel joy is a key trait of depression that can be seen in all types of depression. Even masked depression can be identified by this trait.
Masked depression is depression that runs in an implicit form and masquerades as other illnesses and pains. Sometimes people with these hidden forms of depression go to doctors for a long time until they are referred to a psychiatrist.
Depressions in general and depressive episodes within BAR have many faces, many course and forms. There are depressions with the most pronounced boredom affect, there are variants in which apathy and lack of motivation to any activity are leading, and there are variants in which anxiety comes to the fore.
It also happens that depression hides behind alcohol or drug addiction. About half of patients with BAR have some kind of addiction. They begin as a way of self-medication.
The main symptoms of depression, usually occur over a period of 2 weeks or more:
- Decreased mood, depressed or longing all day or most of the day for a long time.
- Lack of joy, absence of positive emotions and satisfaction from things that were recently pleasurable.
- Fatigue, lack of energy, feeling tired, decreased energy, lethargy, weakness.
Other symptoms that make you suspect depression:
- Bawdiness, irritability, anxiety.
- Lack of desire to go out with friends, desire for privacy, being alone.
- Sleep disorders. Difficulties with falling asleep, early awakening several hours before the usual time, or conversely, the constant sleepiness and too long a dream in comparison with the usual norm.
- Uncomfortable, squeezing or painful feelings in the chest, in the solar plexus area.
- Lowered self-esteem, feelings of guilt, worthlessness, self-blame.
- Gloomy vision of the future, hopelessness, hopelessness.
- Headaches or other painful feelings.
- Difficulty making decisions, difficulty concentrating, feeling stupider than before, slower thinking.
- Lack of appetite or conversely overeating, especially sweets and flour.
- Difficulties in maintaining hygiene and doing household chores.
- Decreased libido.
- Thoughts of death or suicide.
As you can see, the symptoms and manifestations of depression are quite numerous, but they do not all appear at once. Depression most often unfolds over several weeks. As the depressive state becomes more severe, more symptoms may appear, and the severity of these symptoms also increases.
Degrees of severity of depression
In the current version of the ICD-10 disease classification, a depressive episode has several degrees of severity:
- Mild degree depressive episode
- Moderate degree depressive episode
- A depressive episode of severe severity without psychotic symptoms
- Severe depressive episode with psychotic symptoms
With mild depression, the person retains his or her ability to work and may even go into work with his or her head so as not to think about bad things. As the symptoms worsen, the person finds it increasingly difficult to perform work duties and cope with household chores. In the middle stage of depression, the person already refuses to do both work and household chores. And with severe depression, the person has difficulty getting out of bed and, in extreme cases, refuses to drink or drink at all.
Mild Depressive Episode
The first complaints of a depressed person may be somatic problems - headaches, constant feeling of fatigue, rapid fatigue. The person may not yet notice changes in mood. There may be difficulties in decision-making, difficulty in concentrating and thinking. Outwardly, a person with mild depression looks as well as usual.
Then irritability or tearfulness, slight anxiety or apathy gradually join. A sense of joy and interest disappears. There is a sense that there is less energy, the person feels more lethargic and has to make more effort to maintain the same pace of life.
At this stage, all manifestations are not yet deep and total, and the person mostly feels better in the evening. And the number of symptoms of depression is still relatively small, which allows the person to carry out basic activities.

Over time, small disorders of sleep and appetite and a feeling of bodily discomfort appear. As depression worsens, feelings of anxiety and homesickness may appear.
Outwardly, mild depression is almost completely silent. The person may appear as normal.
Moderate Depressive Episode
Also called moderate depression. Four or more symptoms of depression are expressed.
At this stage, the depressed mood is clearly evident - feelings of longing, anxiety and a pessimistic assessment of the future appear. The person already experiences great difficulty in continuing normal activities.
Sleep and appetite disorders are already of a more steady character. Moreover, sleep disorders may be in the direction of insomnia or early awakening (the person wakes up 2-3 hours earlier) and in the direction of oversleeping. In some cases, a person may sleep up to 20 hours a night. Also with appetite, it either disappears or becomes elevated.
The person himself or herself already feels this condition to be more severe. Changes can also be seen in the person's appearance. Movement and facial expressions become slower, and the person looks tired and depressed. Even to an outside observer, the lack of energy, desires, and a constant feeling of fatigue are clearly visible.
"Judging by his words, he has been ill since about the spring of 1905; here he became bored and began to be bored. He has been in the local hospital since September, and it is evident that he is depressed, depressed, and has a sad look. He answers questions quietly, and if he is not asked, he will remain silent. Complains of homesickness: thinks he may not be at home. Sometimes cries for a long time, saying that he has homesickness; usually secludes himself, at times walking a lot, silently and with a sad look." On Melancholy. Clinical Lectures, S. A. Sukhanov. 1906 г.
Experiences during depression can be varied, it is felt as bodily discomfort, longing, restlessness, unaccountable anxiety, sometimes it is felt as absence of emotion. Apathy, indifference, a person feels listless and incapable of action are quite palpable.
At this stage, there are already distinct thoughts of worthlessness and a pessimistic assessment of the future. People are almost completely focused on painful experiences. It can be quite difficult to distract them. There is a loss of desire to communicate and have contact with other people.
In moderate depression, a person experiences great difficulty in performing social duties, household chores, and continuing to work.
The depressed mood fluctuates little during the days, and often there is no reaction to the surrounding circumstances, but there can be characteristic diurnal fluctuations, when the mood slightly improves by the evening.
Severe depressive episode without psychotic symptoms
"I remember her curled up in a tight ball on the couch in our friend's apartment, shuddering as if she had bamboo chips driven under her fingernails. We didn't know what to do. It was as if she was speechless; when we finally squeezed a few words out of her, they were barely audible. Fortunately, her parents had studied bipolar disorder thoroughly over the years, and that night we helped her move in with them. That was the last we would hear from her for two months: she lay in a corner, not moving for days at a time." Andrew Solomon, Noon Demon
During a severe depressive episode, one's consciousness is completely filled with burdensome feelings. A characteristic feature of endogenous depression is atrial longing--a physical sensation of longing in the chest, heart, or solar plexus--is felt constantly. This longing is similar to physical pain, and can be described as a feeling of constriction, petrification, as a feeling of unbearable suffering. These sensations are very intense, and because of this intensity and severity, they command the entire attention. The mind rushes around in a vicious circle of grievous sensations. The diurnal fluctuations of mood characteristic of the lighter stages disappear.
Together with melancholy, anxiety may be felt, and the loss of the ability to feel and communicate normally may also be felt.
Outwardly, a person in such a condition is not difficult to recognize. They rarely get out of bed, they move slowly, speak softly, their lips are dry, facial expressions are either absent or reflect suffering, or they speak quietly or not at all.
Hypochondriacal ideas may develop.
"This stage of the seizure can pass imperceptibly into delusional melancholy, when tragic "clarity" in the patient's consciousness sets in. The distance between the patient's former self and the experienced state has disappeared. The melancholic delirium, in its entirety, expresses in its multiple manifestations the revolution in the patient's self-awareness that has occurred. The former self does not exist now, nor in the past, nor in the future. The external world registered by perception is inaccessible to the patient. All norm (health, wholesomeness, ability to live among people) is inaccessible. He can only hinder by his presence among people; he has been incomplete, unhealthy, sinful before. Death by disease, isolation or punishment is the only and natural prospect." T.F. Papadopoulos, Acute Endogenous Psychosis
People who have experienced a severe depressive episode recall it as one of the worst experiences of their lives:
"I'll never let that happen again," she has told me ever since. - I know I will do anything to avoid it. I absolutely refuse to bear it." .... Andrew Solomon, Noon Demon
During a severe episode, people are usually unable to carry out domestic, social and work activities. Suicides are especially dangerous in or on the way out of severe depression, when the mood is still depressed but the strength is already there.
Severe depressive episode with psychotic symptoms
Psychotic depression is characterized by psychomotor retardation - the person moves slowly, almost does not talk, lies in bed most of the time. This lethargy makes all communication and self-care impossible. Suffering is seen as payment for guilt or sins. While the person's condition is obviously severe, he or she loses all criticism. In such a condition, the person is unaware of the need for treatment.
"A severe depressive episode may be supplemented by delusions, hallucinations or a depressive stupor. Delusions more often have the facet of sinfulness, impoverishment, impending misfortunes for which the patient is responsible. Auditory hallucinations are usually in the form of accusing or abusive voices; olfactory hallucinations are in the form of smells of decaying filth or flesh. Severe psychomotor retardation may progress to stupor." Federal clinical guidelines for the diagnosis and treatment of bipolar affective disorder in adults. Mosolov S.N., Kostyukova E.G., Tsukarzi E.E. November 2013
Hypomania (hypomanic episode)
Hypomania is a mild degree of mania and is characterized by symptoms of mania, but they are less pronounced. A diagnosis requires the presence of 3 to 4 major symptoms over a 4-day period:
- Increased activity or physical restlessness;
- Heightened talkativeness;
- difficulty concentrating or being distracted;
- decreased need for sleep;
- increased sexual energy;
- minor binge eating or other types of reckless
- irresponsible behavior;
- Increased sociability or familiarity
Hypomania is characterized by a constant light upswing in mood, increased vigor and activity, and a feeling of alertness and well-being. An increase in the general tone is characteristic, mental processes run easily, and it is very difficult to darken a person's mood in this state and the world is seen in rosy color.
During hypomania, increased sociability, talkativeness and an increased libido are also noted. The need for sleep decreases. Manifestations of hypomania, as a rule, do not lead to disruptions in work and do not lead to social maladjustment. Sometimes, on the contrary, they can even lead to increased productivity, and the person in hypomania seems interesting, pleasant, enthusiastic, etc. to others.
Feelings of complete well-being and optimism are often disproportionate to the person's reality and abilities. Despite this discrepancy, productivity often does increase, and periods of hypomania are often accompanied by creative activity. It has long been observed that there is a connection between hypomania and the capacity for creativity.
Sometimes, especially with hyperthematic accentuation, the symptoms of hypomania can be difficult to distinguish from the person's inherent normal personality traits. Quite often, though, the person is still aware of some of the unusualness of the changes that are occurring to him or her.
In some cases, instead of increased mood and sociability, irritability and rude behavior may appear.
At the beginning of hypomania, the person usually easily maintains concentration on the activity in which he is interested. He sleeps less and rests less.
But as the condition develops, this ability may be lost, and high concentration is replaced by active switching between interests and activities.
In this condition, it is difficult for the person to admit that there is something wrong with him or her - he or she is in a good mood, he or she is awake and has a lot of time.
However, hypomania is unpredictable; it can last for several hours or days, it can last for several months, or it can be a precursor to the onset of mania. As mania progresses, the ability to criticize is lost.
Manic episode
In its classic version, mania is the opposite of depression and manifests itself in an elevated mood, accelerated thought processes, and increased motor activity. It leads to an unrelenting thirst for activity, a desire to socialize, and disinhibited reactions.
The manic episode begins with a sense of well-being and a good, often carefree and cheerful mood; gradually the mood rises to the level of euphoria and almost uncontrollable excitement. In some cases, the change in mood is expressed not in its elevation, but in irritability and even anger, in these cases we are talking about so-called manic anger mania.
During a manic episode, the need for sleep decreases and sleep seems a waste of time. The desire for activity, on the contrary, increases; at the beginning of the episode, this activity seems productive, but gradually loses effectiveness and becomes chaotic. This happens because of accelerated thinking and high distractibility, the ability to concentrate decreases, and sometimes the person is unable to keep attention on the topic of the conversation or his or her activity for long. Started affairs are not brought to an end.
The person is full of optimism, feels a burst of energy, and the future is seen only in a positive light. Speech becomes fast and loud. Thoughts also fly with great speed, in some cases reaching the "leap of ideas", when the external observer can no longer keep track of the flow of thoughts and associations.
The ability to control one's actions gradually comes to naught. Criticism to his condition also disappears, sometimes the person understands that something is going on with him, but does not attach importance to it.
The first episode of mania often occurs between the ages of 15 and 30, but can be any age from childhood to 70 or 80.
To be diagnosed, the episode must last at least 1 week and be of such severity that it results in impairment of normal functioning and social activities.
Manic episodes develop much more rapidly than depressive episodes, sometimes starting suddenly, lasting from 2 weeks to 5 months (average length of episode is 3-4 months). Manic episodes occur less frequently than depressive ones and last on average shorter.
In a manic state, the person tends to start implementing his ideas immediately, practically bypassing the stage of criticism. If someone tries to interfere or get in the way, it causes irritation and often leads to conflicts. At the same time, initiated cases, whether it is a work project or cleaning in the house, are not completed, the person is switched to another activity. A person in a manic state is almost incapable of being idle or unmoving.
"One of the important features of mania is the tendency to make serious and dangerous decisions quickly. In the lives of people suffering from manic-depressive disorder, unexpected decisions often occur and are immediately realized. Examples include a sudden move abroad, borrowing a large sum of money, a drastic change in the type of activity, or radical decisions in one's personal life (divorce or starting a new relationship). But it is important to emphasize that sometimes in people with special intellectual potential and a propensity to engage in specific activities, an increased willingness to take risks (provided there are no manifestations of disorganized behavior) can lead to high results." Janusz Rybakowski, Faces of Manic Depressive Disorder.
Because of the desire for impulsive, thoughtless action, people in mania do things they regret later-they easily have sexual relations with strangers, use alcohol and drugs, may rashly quit their jobs, leave their family, take out huge loans and start a new project, sell apartments, give away possessions and give away money, move to another country, and so on. People in mania tend to underestimate risks, may drive at high speeds without having time to keep their eyes on the road.
All this is done without delay, and the person tends to overestimate his capabilities and lose criticality of the situation, which he then regrets when he comes to his usual state. After the episode is over, the person often feels a sense of shame and guilt.
"I was aware of what was happening to me. But at the time I was dating a girl who talked me out of going back on the pills. And when the mania started to take full force, there was nothing I could do about it. My head was completely swept away, and I lost control of myself. It seems to me that mania exaggerates a person's personal traits, good or bad. For me, mania is a state in which I feel no risk. I would call it an "uncritical state." I am an outgoing and open person, kind, and it has been abused. I've been taken advantage of, pulled money out of me. One of these dishonest people turned out to be an ex-girlfriend herself. Taking advantage of my inadequate condition, she extorted more than one hundred thousand, and then she even withdrew money from my account. I lived in her kitchen, slept on an air mattress, and spent huge sums on her. I left her when I couldn't even explain myself anymore. After that incident my world was overturned, I could not understand how a person I loved could do such a despicable thing. The result of the new mania was a new debt of 4.2 million rubles. Only after the second mania I fully accepted the fact that I was sick and that I had to take my medication constantly. I started taking pills strictly as recommended by my doctor." Masha Pushkina, How bipolar people live and dream
The main symptoms of mania are
- Increased mood, sense of well-being, productivity, euphoria.
- Increased motor activity, vigor. Activity is usually aimed at achieving some goal - educational, recreational, sexual, social or occupational.
- Reduced need for sleep (a person needs only 3-4 hours, in some cases he/she may not sleep for several days).
- Emotional excitement.
- Accelerated thinking and rapid speech, quick broad gestures (compared to a person's normal gestures). Feeling of leaping thoughts or speeding up the thinking process.
- Increased talkativeness, talkativeness, sociability. Lack of a sense of distance and verbal pressure in relationships with others.
- Decreased normal social control, leading to behavior that is inadequate to the circumstances. Reckless or reckless behavior, the consequences of which the patient is not aware, such as binge eating, inadequate enterprise, reckless driving, ease of entering into sexual relations with strangers.
- Increased self-esteem or ideas of grandiosity (grandiosity).
- Distractibility or constant changes in activities or plans.
Other symptoms of mania
- Attention disorder: increased distractibility.
- Increased irritability or conflict, aggressive behavior.
- Overestimation of own personality and tendency to grandiose ideas.
- Heightened sexuality.
- A marked increase in sexual energy or sexual promiscuity.
- Craving for thrills.
- Monetary spending, credit, shopping.
- Excessive entrepreneurialism, activity, with a large number of things to do, productivity decreases, to the point of complete chaos.
- Unusual creative drive.
- Delusions and hallucinations may develop.
- Rapid, abrupt changes in mood - an elevated mood is replaced by irritability, especially when the person encounters an objection.
During mania, perceptual disturbances may occur, such as experiencing color as especially bright and beautiful. Similar to depression (only in reverse), distorted perceptions of self arise. From increased arrogance at the beginning of the episode, to a sense of omnipotence and a special divine chosenness. Then delirium and hallucinations can join.
"I was 18 when my heart first stopped. An overdose in a club. I don't remember that moment, I was told later that I started throwing myself at people. But my brain wasn't working at that moment, I was unconscious, although my body was moving on its own. I woke up three days later in intensive care in Kupchino. Then I was in narcology for two weeks, but doctors did not understand what was wrong with me and they let me go. I had already been kicked out of the dormitory and had nowhere to go. I wandered the streets, went to the FSB and the police, behaved inadequately, and eventually ended up in Psychiatric Hospital No. 2."
Mania with psychotic symptoms
Increased self-esteem and ideas of grandeur can develop into delusions, and irritability and suspiciousness can develop into delusions of persecution. The surges of thoughts and speech pressure result in the person's speech becoming poorly understood.
In some cases of psychotic mania, people hear voices or see hallucinations.
"Psychotic symptoms can be congruent with affect and noncongruent. Psychotic symptoms congruent with affect are, for example, manic delusions of grandeur, special origins, or "voices" informing the patient of his "superhuman abilities," etc. Non-congruent - may include affectively neutral hallucinations, attitudinal delusions without elements, delusions of meaning or persecution, 'voices' talking to the patient about events that have no emotional significance, etc." Federal clinical guidelines for the diagnosis and treatment of bipolar affective disorder in adults. Mosolov S.N., Kostyukova E.G., Tsukarzi E.E. November 2013.
Mixed condition
"After the death of a close friend, another phase was added to my calendar. This phase was particularly difficult to catch, and it took almost a month before I went to the doctor: on the one hand I slept four hours a night, and on the other I was in a disgusting mood, on the one hand I had lots of energy, and on the other I didn't want to do anything. Neither for the beginning of depression nor for the beginning of hypomania, there seemed to be no reason to turn, until I realized that a month's sleep of 4 hours was not normal after all."
A mixed state can occur when one phase transitions to another, but it can also be an independent phenomenon. Mixed states can account for up to 30% of all affective phases.
A mixed affective episode is characterized by the simultaneous coexistence of hypomanic/manic and depressive symptoms lasting at least 2 weeks, or their rapid (within hours) alternation.
There are many variants of the mixed state:
For example, a sudden burst of vivacity and cheerfulness during a depressive episode and then a return to depression, or conversely a sudden drop in mood and activity during a manic episode.
If manic and depressive symptoms exist simultaneously, symptoms of one pole are replaced by symptoms of the other pole. Inhibited mania and hyperactive depression arise.
There may be a depressed mood along with high energy and a feeling of bursting with energy. Feeling of nothingness, together with a feeling of omnipotence. This condition is sometimes easily confused with agitated depression, but in either case, it requires the intervention of a doctor.
The disorders can be rather pronounced, which leads to considerable social and professional maladjustment.
With a mixed condition, hyperactivity, insomnia, and often psychotic features and suicidal thoughts are noted. Mixed states are usually accompanied by general emotional instability.
During a mixed state, people equally experience agitation, internal restlessness, dejection, and depression. It is because of this combination of increased activity and depression that these states have a particularly high suicide risk.
Summary
We have reviewed the major phases of bipolar disorder: depressive episode, hypomanic, manic, and mixed.